Author: Nicola Winson, Educational Psychologist
Mental Health
Mental health is often considered to mean the absence of a diagnosed mental disorder. However, the World Health Organisation defines mental health as, “a state of well-being in which an individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to his or her community.”
When this explanation of mental health is taken into consideration, many mothers may find that their mental state is not as healthy as they assumed.
In developing countries, like South Africa, one third to one fifth of mothers experience mental health challenges during pregnancy or after childbirth (WHO, 2008).
Causes of Mental Ill-health
Despite the superpowers of mothers, no one is immune to the experience of mental health challenges. Mental health may be influenced by a variety of different factors. Environmental events, such as the current COVID-19 pandemic, transitional phases, for example, moving house or changing jobs and interpersonal relationships, like a marriage, divorce, birth of a child or loss of a friend or relative may have a negative impact on a person’s mental health.
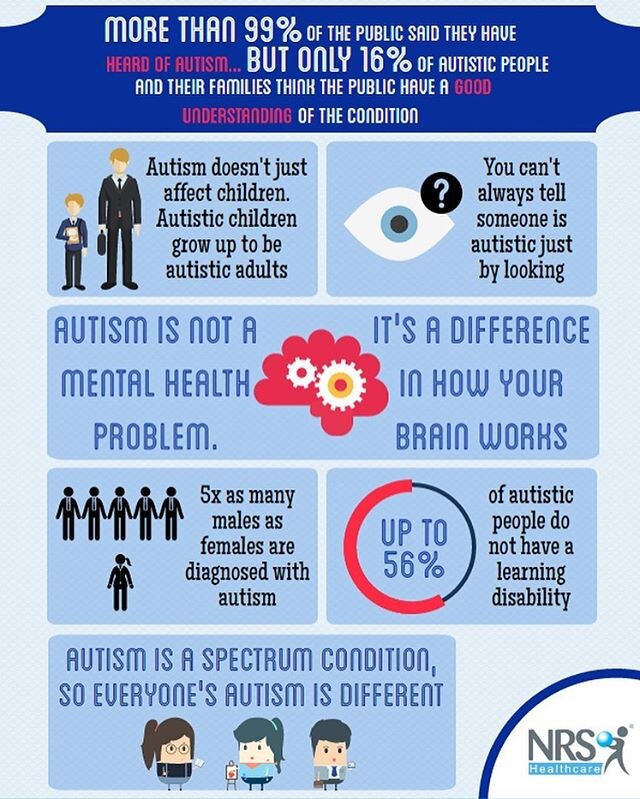
Additional negative influences on mental health include difficulties within social support systems, for example family discord or community violence, a chronic illness or disability or the experience of victimization of any sort. Pre-existing mental conditions, such as anxiety or depression, may be heightened through pregnancy and motherhood and conditions such as pre or post-natal depression may develop. The exciting, yet sometimes terrifying and unexpectedly overwhelming journey of motherhood may leave some mothers particularly vulnerable to mental health challenges.
Importance of Maternal Mental Health
A mother facing mental health challenges may experience increased difficulty in meeting her own needs, let alone those of her infant or young child. Maternal mental health can influence the child before it is born, impact on the bonding experience with the infant and reduce the mother’s abilities to provide the emotional support and guidance necessary for the developing child and teenager. The impact of poor maternal mental health can have life-long social, behavioural, emotional and even cognitive impacts on the developing child.
Overcoming Maternal Mental Health Challenges
The snowball impact of lack of sleep, physical discomfort, fluctuating emotions, change in routine and the responsibility of nurturing a new life while juggling other relationships may leave mothers feeling overwhelmed, anxious or despondent. However, mothers encountering these and similar challenges are not required to face their struggles alone. The strength of a supermom is proportionate to her ability to ask for help when needed. Interaction with support groups, a counsellor or psychologist can assist mothers with developing coping strategies, gaining greater self-insight and sharing the emotional load of motherhood. Through obtaining the necessary support, mothers are able to improve not only their own mental health but also that of their children.
References
Barlow, J., McMillan, A. S., Kirkpatrick, S., Ghate, D., Barnes, J., & Smith, M. (2010). Health‐led interventions in the early years to enhance infant and maternal mental health: A review of reviews. Child and Adolescent Mental Health, 15(4), 178-185.
Hogan, R. (2019). Maternal health. Salem Press Encyclopaedia
Phua, D. Y., Kee, M. Z., & Meaney, M. J. (2020). Positive maternal mental health, parenting, and child development. Biological Psychiatry, 87(4), 328-337.
World Health Organisation. (2008). Maternal mental health and child health and development in low and middle income countries. Report of the WHO meeting. Geneva.
https://www.who.int/mental_health/maternal-child/maternal_mental_health/en/
https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
https://wmmhday.postpartum.net/
Photo 1: Andrea Lightfoot on Unsplash
Photo 2: Caroline Miller Photography. Permission given by model.